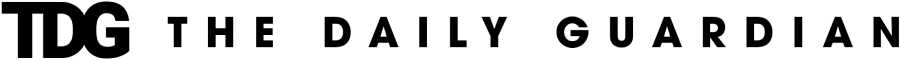
Smoking has long been linked to various cancers and blood disorders, but recent studies have uncovered a significant connection between smoking and the development of myelodysplastic syndromes (MDS). Myelodysplastic syndromes are a group of hematologic (blood) conditions characterized by the abnormal production of blood cells. This leads to ineffective hematopoiesis (blood cell formation) and a higher risk of progression to acute myeloid leukemia (AML), a more aggressive form of blood cancer. While genetic mutations are known to play a central role in the pathogenesis of MDS, recent research highlights smoking as a major environmental risk factor that accelerates the accumulation of genetic mutations in MDS patients, increasing their risk of progression to leukemia.
Understanding Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes are a group of hematologic disorders that cause the bone marrow to produce insufficient and abnormal blood cells. These syndromes often result in low counts of red blood cells (anemia), white blood cells (leukopenia), and platelets (thrombocytopenia), which can lead to a variety of symptoms including fatigue, frequent infections, and bleeding. MDS can occur de novo (without any prior blood disorders) or as a secondary condition, often following treatment for other cancers, such as chemotherapy or radiation therapy. In some cases, MDS can transform into acute myeloid leukemia (AML), which significantly worsens the prognosis.
The Role of Genetic Mutations in MDS
Genetic mutations play a crucial role in the development of MDS. These mutations often affect genes involved in cell differentiation, apoptosis (programmed cell death), and cell cycle regulation. As a result, abnormal blood cells are produced, which accumulate in the bone marrow and fail to mature properly. Over time, this leads to ineffective hematopoiesis, making it difficult for the body to produce healthy blood cells.
Several mutations have been identified in MDS, including mutations in the TP53 gene (which is involved in tumor suppression), the ASXL1 gene (which regulates gene expression), and the DNMT3A gene (which plays a role in DNA methylation). These mutations are often associated with poor prognosis and a higher likelihood of progression to AML. However, not all patients with MDS develop these mutations, and the specific genetic makeup of the disease can vary widely between individuals.
Smoking and Its Impact on Genetic Mutations
Smoking is known to cause genetic damage through the introduction of carcinogens into the body. The inhalation of tobacco smoke releases a variety of toxic chemicals, including polycyclic aromatic hydrocarbons (PAHs), nitrosamines, and reactive oxygen species (ROS). These substances can directly damage the DNA in cells, leading to mutations that accumulate over time. Smoking is strongly associated with several types of cancers, including lung cancer, head and neck cancers, and esophageal cancer, but recent studies have also pointed to smoking as a significant risk factor for the development of MDS.
Several studies have shown that smoking accelerates the accumulation of genetic mutations in the bone marrow, which may lead to the development of MDS. The genetic damage caused by smoking often targets genes involved in cell cycle regulation, DNA repair, and apoptosis. This makes the cells more likely to proliferate abnormally, contributing to the development of hematologic disorders like MDS. One of the key mechanisms by which smoking induces genetic mutations is through the formation of DNA adducts—covalent bonds between the DNA and carcinogens—which can result in mispairing of nucleotides during DNA replication, leading to mutations.
Studies Linking Smoking to MDS
A growing body of research has begun to link smoking to the development and progression of MDS. One study conducted by researchers from the Mayo Clinic found that smoking was a significant risk factor for the development of secondary MDS, particularly in patients who had previously received chemotherapy or radiation therapy for other cancers. The study found that smoking significantly increased the risk of genetic mutations in genes associated with MDS, especially those involved in DNA repair and cell cycle regulation.
In another large cohort study, researchers found that smoking was associated with an increased risk of developing MDS in a group of older adults. The study showed that smokers had a higher prevalence of mutations in key genes involved in hematopoiesis, including TP53 and ASXL1, compared to non-smokers. Additionally, smokers were more likely to have a more aggressive form of MDS, with a higher risk of progression to AML.
These findings suggest that smoking not only increases the risk of developing MDS but also accelerates the progression of the disease by contributing to the accumulation of genetic mutations. This is particularly concerning for patients who have already been diagnosed with MDS, as the presence of additional mutations could make the disease more difficult to treat and increase the likelihood of treatment resistance.
Mechanisms Behind Smoking-Linked Genetic Mutations in MDS
The mechanisms by which smoking leads to genetic mutations in MDS are complex and multifactorial. One of the main contributors is the carcinogenic effects of the chemicals found in tobacco smoke. These chemicals can bind to DNA and form adducts, which cause errors during DNA replication and repair. Over time, these errors accumulate, leading to the formation of mutations in critical genes involved in cell growth and survival.
One of the key genes affected by smoking-related mutations in MDS is TP53. TP53 is a tumor suppressor gene that helps prevent the growth of abnormal cells by inducing cell death when DNA damage occurs. Mutations in TP53 are common in MDS and are often associated with a poor prognosis. Smoking has been shown to increase the frequency of TP53 mutations, making it more difficult for the body to control the growth of abnormal blood cells.
In addition to TP53, other genes involved in DNA repair, such as DNMT3A and ASXL1, are also frequently mutated in MDS patients who smoke. These genes play crucial roles in maintaining the integrity of the genome, and mutations in these genes can result in the loss of normal cell cycle regulation, leading to the proliferation of mutated cells.
Implications for MDS Treatment
The discovery of the link between smoking and genetic mutations in MDS has important implications for the treatment and management of the disease. Patients who smoke or have a history of smoking may have a higher burden of genetic mutations in their bone marrow, which could make their MDS more difficult to treat. For example, patients with mutations in TP53 or other key genes may have a poorer response to standard treatments like chemotherapy or stem cell transplants, as these therapies rely on the ability of the patient’s immune system to recognize and eliminate abnormal cells.
Additionally, the presence of smoking-related mutations may contribute to resistance to newer targeted therapies that aim to block specific mutations or signaling pathways in leukemia cells. Therefore, understanding the genetic makeup of MDS patients, including whether smoking has contributed to the accumulation of mutations, is essential for selecting the most effective treatment options.
Preventing Smoking-Related MDS
Given the strong link between smoking and the development of genetic mutations in MDS, smoking cessation is an essential preventive measure for reducing the risk of the disease. Public health campaigns aimed at reducing smoking rates and increasing awareness of the risks associated with tobacco use can play a significant role in preventing MDS and other tobacco-related cancers. Healthcare providers should encourage patients to quit smoking, especially those with risk factors for MDS, such as a family history of blood cancers or previous cancer treatments.
Smoking is a well-known risk factor for a variety of cancers and diseases, but its role in the development of myelodysplastic syndromes (MDS) and the accumulation of genetic mutations is becoming increasingly clear. Smoking accelerates the genetic mutations that lead to MDS, contributing to the development of abnormal blood cells and increasing the risk of progression to acute myeloid leukemia (AML). As research continues to uncover the molecular mechanisms behind smoking-related mutations, it is important to emphasize the need for smoking cessation as a preventive measure and consider smoking history when diagnosing and treating MDS patients. Ultimately, addressing smoking as a major environmental risk factor for MDS will be critical to improving patient outcomes and reducing the burden of this serious hematologic disorder.