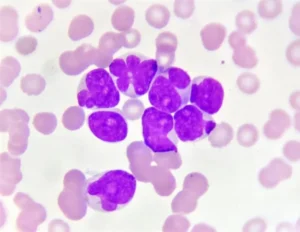
Recent advancements in leukemia treatment have brought promising results with the development of triplet therapies for both relapsed and newly diagnosed cases. These therapies combine three different classes of drugs to target leukemia from multiple angles, improving efficacy and potentially offering better survival outcomes for patients. Leukemia, a form of blood cancer, has long been a challenging disease to treat, with treatment options often limited to chemotherapy, radiation, and stem cell transplants. However, the emergence of triplet therapies marks a significant leap forward in the precision treatment of this malignancy.
The Challenge of Leukemia Treatment
Leukemia, particularly acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL), remains a significant global health concern. Despite the availability of traditional therapies, a considerable number of patients either do not respond to treatment or experience relapse after initial remission. This is especially true for older patients or those with complex genetic mutations. The need for more effective therapies is clear, as the standard treatments often result in toxic side effects and can be ineffective for certain subtypes of leukemia.
Current treatment strategies primarily involve chemotherapy, which can lead to remission in many patients, but it is not always a durable solution. Chemotherapy targets rapidly dividing cells, but leukemia cells can adapt and evolve, leading to drug resistance. Additionally, chemotherapy often damages healthy cells, resulting in severe side effects. Bone marrow transplants offer another option, but they come with significant risks and complications, particularly in older patients or those with comorbidities.
Enter Triplet Therapy
Triplet therapy involves the combination of three different drugs that work together to target the leukemia from various biological and molecular pathways. These therapies are designed to be more effective and less likely to provoke resistance compared to traditional two-drug regimens. By attacking leukemia on multiple fronts, triplet therapies aim to overcome the ability of the leukemia cells to evade treatment and potentially improve survival rates, particularly in patients who have relapsed after previous treatments.
The idea of combining multiple drugs is not new in oncology, but the specific approach for leukemia has seen significant evolution in recent years. A triplet therapy regimen may involve chemotherapeutic agents, targeted therapies, and immunotherapies. The goal is to simultaneously address both the cancerous cells and the factors that allow them to thrive, including their microenvironment and immune evasion mechanisms.
Triplet Therapy in AML
Acute myeloid leukemia (AML) is one of the deadliest types of leukemia, characterized by the rapid proliferation of immature blood cells. It is often associated with poor prognosis, particularly in elderly patients or those with high-risk genetic mutations. The treatment landscape for AML has traditionally been dominated by chemotherapy, with regimens such as “7+3” being the standard of care. However, despite initial responses, relapses are common, and long-term survival rates remain low.
Recent studies have shown that triplet therapies can offer a more robust solution for AML patients, particularly those with relapsed or refractory disease. One promising combination involves adding targeted therapies such as venetoclax, a BCL-2 inhibitor, to a backbone of chemotherapy and a hypomethylating agent like azacitidine. This combination has demonstrated significant improvements in remission rates and survival outcomes in clinical trials. Venetoclax works by inhibiting a protein that prevents cancer cells from dying, allowing for greater susceptibility to the other drugs in the combination.
In addition to venetoclax, researchers are investigating the use of immune checkpoint inhibitors and other molecularly targeted agents in combination with chemotherapy. These drugs work by restoring the immune system’s ability to recognize and attack cancer cells, which is crucial in overcoming the resistance mechanisms that leukemia cells often develop.
Triplet Therapy in CLL
Chronic lymphocytic leukemia (CLL) is another common form of leukemia, characterized by the slow accumulation of malignant B lymphocytes. CLL typically affects older adults, and while it is a more indolent form of leukemia, it can still present significant challenges when it comes to treatment. Many patients with CLL experience relapses after initial treatment, making the disease difficult to manage over time.
For CLL, triplet therapy regimens have also shown promise, particularly in patients who have relapsed or are treatment-naive. A well-known triplet combination includes a Bruton’s tyrosine kinase (BTK) inhibitor like ibrutinib, an anti-CD20 monoclonal antibody such as rituximab, and a chemotherapy agent like fludarabine. This combination targets the leukemia cells from different angles: the BTK inhibitor blocks signaling pathways that are critical for cancer cell survival, while the anti-CD20 antibody targets the surface proteins of the malignant cells for immune-mediated destruction.
Clinical trials investigating triplet regimens in CLL have shown that this combination can achieve high response rates, even in patients with high-risk features or those who have failed previous treatments. The introduction of targeted therapies like ibrutinib has transformed the treatment landscape for CLL, but combining it with other agents in a triplet regimen may further improve outcomes.
Mechanisms of Action
The success of triplet therapies in leukemia is largely attributed to the way these drugs complement each other and target multiple mechanisms that leukemia cells use to survive and proliferate. For example, chemotherapy kills rapidly dividing cells, but leukemia cells can often develop resistance by altering their DNA repair mechanisms or by upregulating survival proteins. Targeted therapies like venetoclax and ibrutinib block the proteins that help leukemia cells evade cell death and immune attack, enhancing the effectiveness of chemotherapy.
In AML, triplet regimens may also include hypomethylating agents, which work by altering the epigenetic regulation of cancer cells, reactivating tumor suppressor genes, and making leukemia cells more responsive to treatment. In CLL, the combination of a BTK inhibitor and an anti-CD20 antibody is designed to disable both the internal survival pathways of the cancer cells and the immune system’s ability to target them, respectively.
Clinical Evidence and Trials
Several clinical trials are underway to investigate the effectiveness of triplet therapies in both newly diagnosed and relapsed leukemia patients. In AML, one major study is exploring the combination of venetoclax with chemotherapy and a hypomethylating agent in elderly or high-risk patients. Early results from these trials have shown promising remission rates and improvements in overall survival, particularly when compared to standard chemotherapy regimens. For CLL, the combination of ibrutinib, rituximab, and fludarabine is being investigated in various trial phases, with early-phase trials demonstrating significant improvements in progression-free survival.
While these triplet regimens show considerable promise, it is important to note that they are not without challenges. The complexity of managing multiple medications, the potential for increased side effects, and the high cost of these treatments are factors that need to be carefully considered. However, the potential benefits in terms of improved survival and quality of life may outweigh these challenges, particularly for patients with relapsed or refractory leukemia who have limited treatment options.
The Future of Triplet Therapies
The future of triplet therapies in leukemia treatment looks promising. As our understanding of the molecular and genetic underpinnings of leukemia improves, new targets and drugs will likely emerge, further enhancing the potential of triplet combinations. Ongoing research into the optimal combinations, dosing schedules, and patient populations will refine these therapies, ensuring that they are tailored to maximize efficacy while minimizing toxicity.
In addition, as more therapies move from clinical trials to standard clinical practice, the integration of triplet therapies into routine care will require collaboration between oncologists, hematologists, and pharmacists to ensure that patients receive the best possible treatment. Moreover, as precision medicine continues to evolve, triplet therapies may be further personalized to each patient’s unique genetic and molecular profile, offering even greater chances for success.
The advent of triplet therapies in leukemia represents a significant advancement in the treatment of both relapsed and newly diagnosed cases. By targeting the disease from multiple angles, these therapies offer hope to patients who have previously had limited options. While there are still hurdles to overcome, including the management of side effects and the high cost of treatment, the clinical success of these regimens offers promise for improved survival rates and quality of life for leukemia patients. As research continues, it is likely that triplet therapies will become a cornerstone in the fight against leukemia, offering a more effective and durable treatment option for those in need.